Our objective
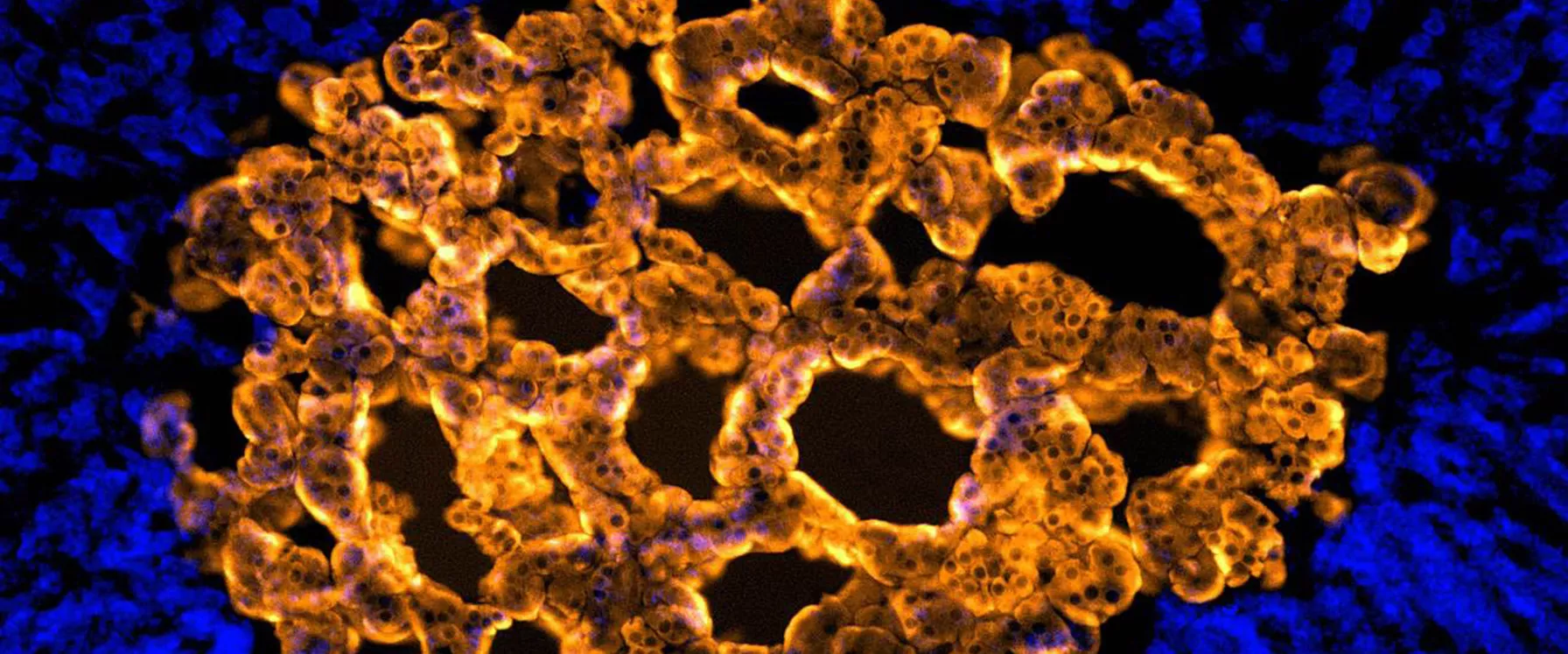
Our mission is to reduce death and disability associated with heart disease by reducing atherosclerotic plaque build-up.
Our research aims to develop novel therapies to target atherosclerosis (arterial blockages) and its consequences (heart attack). Our treatment mission is to develop dedicated agents that specifically target the inflammation that drives coronary plaque instability. Our work is performed in collaboration with the Clinical Research, Vascular Complications and Atherosclerosis and Vascular Remodelling Groups within the HRI, drawing upon their expertise in each area of research.
Our impact
One Australian dies from an acute coronary syndrome (ACS) every 51 minutes. Failure to specifically target persistent coronary inflammation, which drives high rates of recurrent events, is likely a major factor.
To address this problem, our research program’s overarching aim is to: (1) elucidate new inflammatory pathways in ACS patients and (2) re-purpose established anti-inflammatory drugs that target these pathways.
We have focused on colchicine, a safe, cheap and effective anti-inflammatory agent. Our program was the first to show that colchicine has striking athero-protective effects. Our findings are recognised internationally, with 20 papers and 25 presentations (at national and international scientific symposia) in the last five years. Notably, this program’s work has been cited 202 times by groups in 16 countries (Google Scholar), demonstrating its reach. We have also received significant national and international media attention (Sydney Morning Herald, national evening news, TCTmd, heart.org).
Our research identified the potential of colchicine in the treatment of ACS patients.
We developed a safer and more robust technique for sampling blood from the coronary sinus in order to measure trans-coronary cytokine gradients (Martinez et al, IJC 2014). This provided the basis for ongoing studies. In 2015, we showed that a single dose of oral colchicine significantly reduces trans-coronary gradients of key inflammatory cytokines, all of which are highly predictive of future events in coronary artery disease patients (Martinez et al JAHA 2016).
To address mechanism and strengthen research impact, we described monocyte inflammasome activation in ACS patients and how colchicine attenuates this (Robertson et al, Clin Sci 2016). We currently have two papers under review demonstrating inhibitory effects of colchicine on chemokines and miRNA, relevant to inflammation and atherosclerosis.
In 2017, we established a computerised tomography coronary angiography program at Royal Prince Alfred Hospital, resulting in our third major colchicine publication, further strengthening our proposal that colchicine is athero-protective, through plaque stabilisation, independent of statin use (Vaidya et al, JACC imaging 2017). As acute stroke and ACS share common pathophysiologic mechanisms, we recently conducted a meta-analysis of the effects of colchicine on stroke incidence (accepted for publication in Clinical Therapeutics).
Taken together, our work provides compelling mechanistic evidence for a therapeutic role of colchicine in acutely suppressing athero-inflammation, stabilising vulnerable plaque and improving clinical outcomes.
In 2024, we established international network of recruiting sites for COLCARDIO clinical trial, which should significantly boost patient recruitment as well as fostering new international collaborations.
Selected publications
Tucker B, et al. Colchicine as a Novel Therapy for Suppressing Chemokine Production in Patients With an Acute Coronary Syndrome: A Pilot Study. Clinical Therapeutics. 2019; 41 (10): 2172-2181, October 01, 2019.
Kurup R, et al. Neutrophils in Acute Coronary Syndrome. EMJ Cardiol. 2017;5[1]:79-87.
Martínez GJ, et al. Colchicine acutely suppresses local cardiac production of inflammatory cytokines in patients with an acute coronary syndrome. JAHA 2015, 4(8):e002128.
Robertson S, et al. Colchicine therapy in acute coronary syndrome patients acts on caspase-1 to suppress NLRP3 inflammasome monocyte activation. Clin Sci 2016, 130(14):1237-46.
Vaidya K, et al. Colchicine therapy and plaque stabilization in patients with acute coronary syndrome JACC. Cardiovasc imaging, 2017.08.013.
Martínez GJ, et al. The NLRP3 inflammasome and the emerging role of colchicine to inhibit atherosclerosis-associated inflammation. Atherosclerosis. 2017, 269:262-271.
Choteau SA, et al. Transcoronary Gradients of HDL-Associated MicroRNAs in Unstable Coronary Artery Disease. Int J Cardiol. 2018, 253:138-144.
C Khandkar, J Fulcher, S Patel, A Keech. Treatment of vulnerable atherosclerotic plaques: the PREVENT trial. The Lancet 404 (10465). 2024, 1811-1812.
SP Cartland, MS Patil, E Kelland, N Le, L Boccanfuso, CP Stanley. The generation of stable microvessels in ischemia is mediated by endothelial cell derived TRAIL. Science Advances 10 (40), eadn8760
PJ Psaltis, MT Nguyen, K Singh, A Sinhal, DTL Wong, R Alcock, Optical coherence tomography assessment of the impact of colchicine on non-culprit coronary plaque composition after myocardial infarction. Cardiovascular Research, cvae191.
B Tucker, N Goonetilleke, S Patel, A Keech. Colchicine in atherosclerotic cardiovascular disease. Heart 110 (9), 618–625.
Current Research Projects
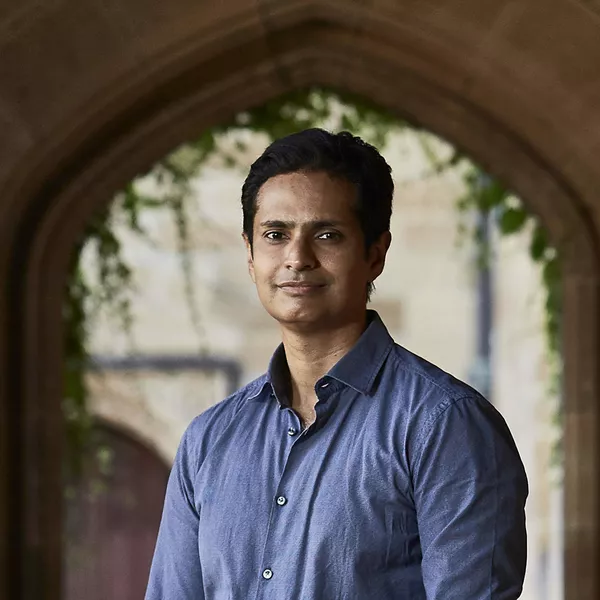
Professor Patel co-leads two large scale MRFF and NHMRC funded clinical trials of colchicine, a safe, well established anti-inflammatory drug in heart attack (COLCARDIO) and stroke (CASPER) survivors. Co-investigators on these studies are national and international leaders in ACS and stroke.
Professor Patel hold senior leadership positions in the following clinical trials/research studies
- MR-CASPER. Brain MRI substudy embedded within CASPER. MRFF funded.
- Colchicine-COG: the effects of low-dose colchicine on cognition and brain health in CAD patients. Sub-study nested within COLCARDIO-ACS. NHF funded, STAR-PAD. NHF funded.
- Aortic & lung Inflammation following COVID, AISRF funded, collaborating with Girish Diwedi (UWA) and All India Institute of Medical Sciences researchers.
- Endothelial Cell Pericyte Crosstalk, NHMRC funded, collaborating with Mary Kavurma from the HRI and Cambridge University.
- Colchicine nanotherapy, NSW Health funded, collaborating with UNSW researchers.
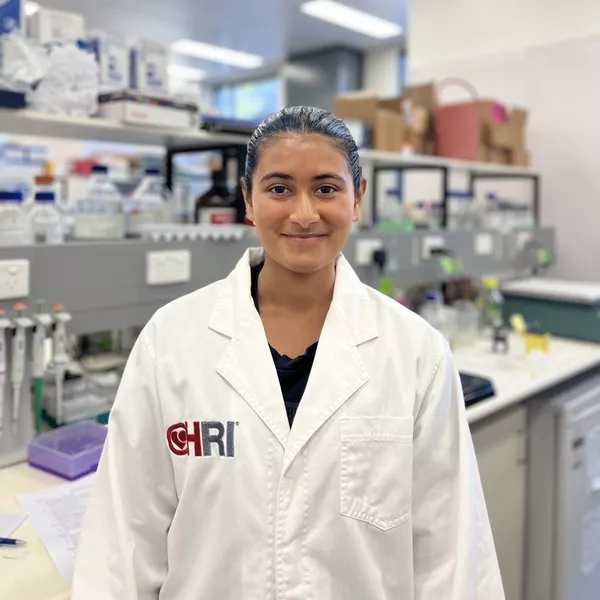
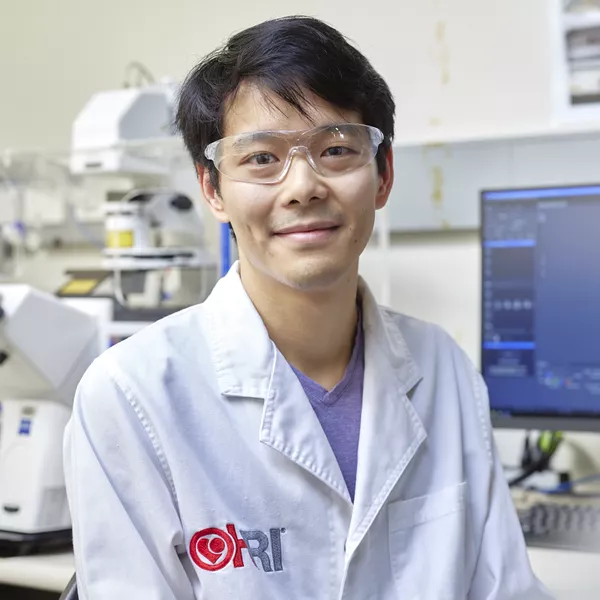
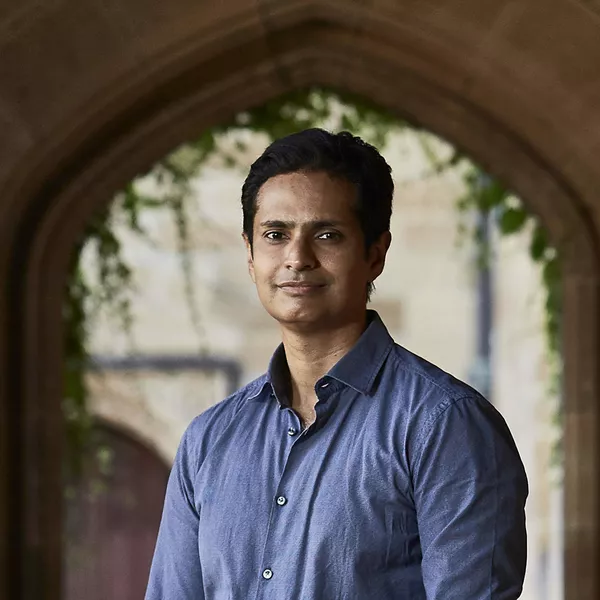
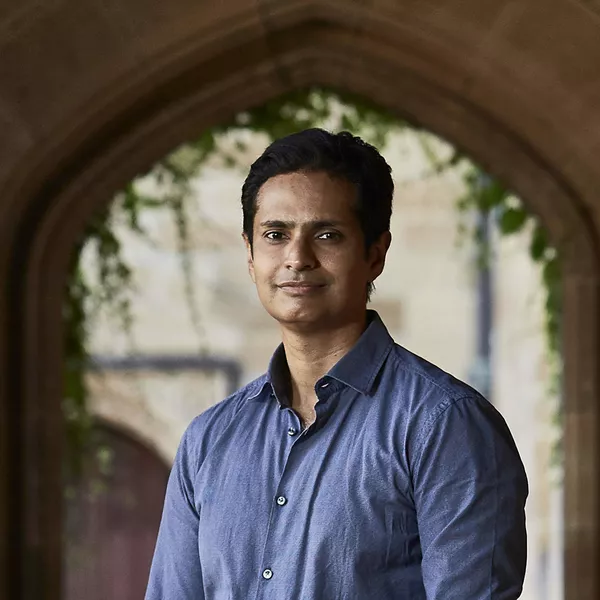
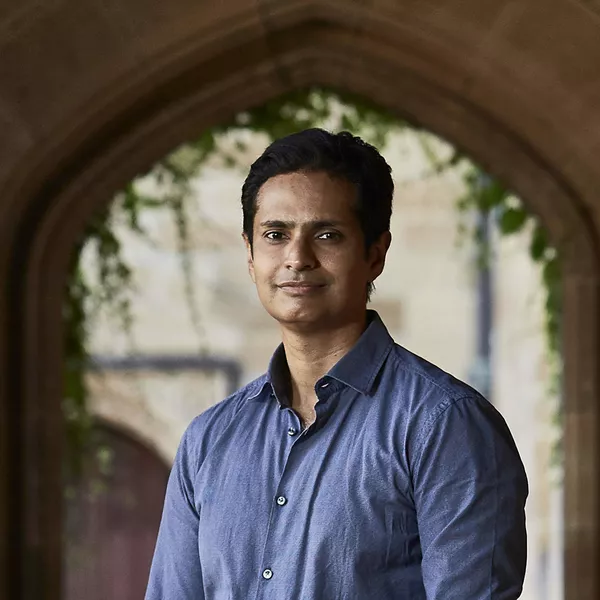
The team
Projects
Determining the effects of colchicine on smooth muscle cell plasticity in advanced atheroma
Determining the anti-atherosclerotic properties of TRAIL
Effects of colchicine on metabolomic profiles in coronary disease patients
Effects of colchicine on miRNA levels in coronary disease patients
Effects of colchicine on prognostically significant vascular endpoints in patients post-acute coronary syndrome (ACS)
Effects of colchicine on neutrophil function in acute coronary syndrome (ACS) patients
Salutary effects of colchicine in a murine model of type 2 diabetes
The effects of colchicine on the development and regression of atherosclerosis
The effects of colchicine on immune cell migration in acute coronary syndrome patients
News
Research assistant Michael Hutton publishes review on atherosclerosis research

HRI reviews colchicine for cardiovascular disease
Associate Professor Sanjay Patel awarded NHMRC grant

Big-hearted investment to save Australian lives
Gout drug mends broken hearts